Progel™ is the only FDA-approved product for adjunctive treatment of pleural air leaks. Progel™ PALS forms a highly-flexible hydrogel specifically designed for use on the lung.
Progel™ Pleural Air Leak Sealant
A unique option designed to address postoperative air leak complications.

- Overview
- EIFU & Resources
- FAQ

- The only sealant specially designed for the lung and its unique characteristics.
- Combines Polyethylene Glycol (PEG) and Human Serum Albumin (HSA) to form a flexible hydrogel.
- Gels at the tissue site, binding directly to the lung for optimal adherence and an airtight seal.
- Strong enough to withstand re-expansion of the lung within 2 minutes of application2,3
- Highly elastic to allow the lung to expand and contract naturally during respiration.
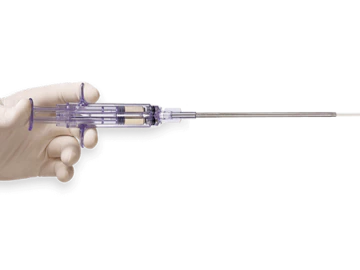
- The patented Progel™ Spray Tip allows for customized application from a single, easy-to-use device.
- The only sealant approved by the FDA to treat pleural air leaks2
- FDA approved to treat air leaks in open thoracotomy, Video-Assisted and Robotic Assisted Thoracic Surgery2
- The only sealant clinically proven to effectively treat air leak complications in both open and minimally invasive thoracic surgery1,2
- Sealed or reduced 96% of air leaks in the OR in a recent clinical trial of patients undergoing Video-Assisted or Robotic-Assisted lung resection2
- Reduced inpatient length of hospitalization by an average of 1.9 days in a prospective, randomized clinical trial1

- As many as 58% of lung surgery patients will have an air leak in the OR1, and more than 15% will develop a persistent air leak after surgery4
- Identifying and treating air leaks intraoperatively provides the best chance for preventing persistent air leak complications and providing incidental cost-of-care savings5
- Progel™ Pleural Air Leak Sealant has been shown to effectively seal air leaks during lung surgery, reducing length of hospitalization by 1.9 days on average, potentially minimizing associated complications and providing cost-of-care savings1
1. Allen, Mark S. et al, “Prospective Randomized Study Evaluating a Biodegradable Polymeric Sealant for Sealing Intraoperative Air Leaks That Occur During Pulmonary Resection” Annals of Thoracic Surgery 2004; 77:1792-1801. Pivotal study. Data on file.
2. Progel™ Pleural Air Leak Sealant Instructions for Use. M-00443. Davol Inc. Data on file.
3. Davol Inc. In Vitro Bench Testing. Data on File. In vitro test results may not correlate to clinical performance.
4. Brunelli et al. Predictors of prolonged air leak after pulmonary lobectomy. Ann Thorac Surg 2004; 77: 1205-1210. Based on the reported incidence of prolonged postoperative air leak.
5. Okereke, I, Murthy, SC, Alster, JM, Blackstone, EH, Rice, TW. Characterization and Importance of Air Leak After Lobectomy. Ann Thorac Surg 2005;79:1167-1173.
6. Estimated based on 4Q 2014 sales data and an estimate of 1.2 mL kits per procedure.
Intended Use / Indications For Use
Progel™ Pleural Air Leak Sealant is a single use device intended for application to visceral pleura after standard visceral pleural closure with, for example, sutures or staples, of visible air leaks incurred during resection of lung parenchyma.
Contraindications
Do not use Progel™ PALS in patients who have a history of an allergic reaction to Human Serum Albumin or other device components.
Do not use Progel™ PALS in patients who may have insufficient renal capacity for clearance of the Progel™ PALS polyethylene glycol load.
Do not apply Progel™ PALS on open or closed defects of main stem or lobar bronchi due to a possible increase in the incidence of broncho-pleural fistulae, including patients undergoing pneumonectomy, any sleeve resection or bronchoplasty.
Warnings
Do not apply Progel™ PALS on oxidized regenerated cellulose, absorbable gelatin sponges or any other surface other than visceral pleura as adherence and intended outcome may be compromised.
Precautions
The safety and effectiveness of Progel™ PALS has not been established in patients with the following conditions:
- Less than 18 years of age, pregnant or nursing women.
- Contaminated or dirty pulmonary resection cases.
- The presence of an active infection.
- In the presence of other sealants, hemostatic devices or products other than sutures and staples used in standard visceral pleural closure.
- Visceral pleural air leak due to spontaneous pneumothorax, any non-resective pulmonary tissue trauma, or malignancy as well as congenital or acquired functional or anatomic defect.
- Patients receiving Progel™ PALS in more than one application session (surgery) before and/or after resorption of Progel™ PALS that was applied in any previous surgical session.
- In any area or tissue other than the visceral pleural surface as indicated.
FEV1 ≤ 40% due to small sample size in the clinical study. In the original pivotal study, all 5 Progel™ PALS and 4 Control patients with FEV1 ≤ 40% had post-operative air leak (POAL); whereas in patients with FEV1 > 40%, 59/93 (63.4%) Progel™ PALS. and 45/53 (84.9%) Control patients had POAL. See Section 7.9 Effectiveness: Primary Effectiveness Outcome in the Instructions for Use.
Adverse Events
In a pivotal clinical trial there were 3 subjects in the Progel™ PALS group with AEs that were considered by the investigator to be possibly or probably related to the device. The AEs reported were: chest pain, constipation, gastroesophageal reflux, nausea, cough, dyspnea, pneumothorax, and subcutaneous emphysema. All were reported as a single occurrence in the Progel™ PALS group. Two of the AEs, dyspnea and chest pain, were reported as “severe” and “serious,” respectively and occurred in the same subject. All others were reported as mild or moderate. In a clinical trial there were reports of renal dysfunction, urinary system disorders and deaths within the study population. None of these have been confirmed to be associated with Progel™ PALS.
In a subsequent minimally invasive clinical trial there were no device related adverse events or unanticipated adverse events. The majority of AEs reported in this study were mild or moderate in severity. The majority of SAEs were pulmonary and expected events as part of a lung resection surgery. Two patients died during the course of the study, one due to cardiac arrest and another due to multi-system organ failure; neither were device related or unanticipated.
The details of these clinical trial adverse events can be reviewed in the IFU supplied with the product an d also available at www.bd.com
Caution: Federal (USA) law restricts this device to sale by or on order of a licensed physician or properly licensed practitioner.
BD-79626
BD offers training resources to help improve your clinical practices as part of our goal of advancing the world of health.
BD supports the healthcare industry with market-leading products and services that aim to improve care while lowering costs. We host and take part in events that excel in advancing the world of health™.
1. Allen, Mark S. et al, “Prospective Randomized Study Evaluating a Biodegradable Polymeric Sealant for Sealing Intraoperative Air Leaks That Occur During Pulmonary Resection” Annals of Thoracic Surgery 2004; 77:1792-1801. Pivotal study. Data on file.
2. Progel™ Pleural Air Leak Sealant Instructions for Use. M-00443. Davol Inc. Data on file.
3. Davol Inc. In Vitro Bench Testing. Data on File. In vitro test results may not correlate to clinical performance.
4. Brunelli et al. Predictors of prolonged air leak after pulmonary lobectomy. Ann Thorac Surg 2004; 77: 1205-1210. Based on the reported incidence of prolonged postoperative air leak.
5. Okereke, I, Murthy, SC, Alster, JM, Blackstone, EH, Rice, TW. Characterization and Importance of Air Leak After Lobectomy. Ann Thorac Surg 2005;79:1167-1173.
6. Estimated based on 4Q 2014 sales data and an estimate of 1.2 mL kits per procedure.
Intended Use / Indications For Use
Progel™ Pleural Air Leak Sealant is a single use device intended for application to visceral pleura after standard visceral pleural closure with, for example, sutures or staples, of visible air leaks incurred during resection of lung parenchyma.
Contraindications
Do not use Progel™ PALS in patients who have a history of an allergic reaction to Human Serum Albumin or other device components.
Do not use Progel™ PALS in patients who may have insufficient renal capacity for clearance of the Progel™ PALS polyethylene glycol load.
Do not apply Progel™ PALS on open or closed defects of main stem or lobar bronchi due to a possible increase in the incidence of broncho-pleural fistulae, including patients undergoing pneumonectomy, any sleeve resection or bronchoplasty.
Warnings
Do not apply Progel™ PALS on oxidized regenerated cellulose, absorbable gelatin sponges or any other surface other than visceral pleura as adherence and intended outcome may be compromised.
Precautions
The safety and effectiveness of Progel™ PALS has not been established in patients with the following conditions:
- Less than 18 years of age, pregnant or nursing women.
- Contaminated or dirty pulmonary resection cases.
- The presence of an active infection.
- In the presence of other sealants, hemostatic devices or products other than sutures and staples used in standard visceral pleural closure.
- Visceral pleural air leak due to spontaneous pneumothorax, any non-resective pulmonary tissue trauma, or malignancy as well as congenital or acquired functional or anatomic defect.
- Patients receiving Progel™ PALS in more than one application session (surgery) before and/or after resorption of Progel™ PALS that was applied in any previous surgical session.
- In any area or tissue other than the visceral pleural surface as indicated.
FEV1 ≤ 40% due to small sample size in the clinical study. In the original pivotal study, all 5 Progel™ PALS and 4 Control patients with FEV1 ≤ 40% had post-operative air leak (POAL); whereas in patients with FEV1 > 40%, 59/93 (63.4%) Progel™ PALS. and 45/53 (84.9%) Control patients had POAL. See Section 7.9 Effectiveness: Primary Effectiveness Outcome in the Instructions for Use.
Adverse Events
In a pivotal clinical trial there were 3 subjects in the Progel™ PALS group with AEs that were considered by the investigator to be possibly or probably related to the device. The AEs reported were: chest pain, constipation, gastroesophageal reflux, nausea, cough, dyspnea, pneumothorax, and subcutaneous emphysema. All were reported as a single occurrence in the Progel™ PALS group. Two of the AEs, dyspnea and chest pain, were reported as “severe” and “serious,” respectively and occurred in the same subject. All others were reported as mild or moderate. In a clinical trial there were reports of renal dysfunction, urinary system disorders and deaths within the study population. None of these have been confirmed to be associated with Progel™ PALS.
In a subsequent minimally invasive clinical trial there were no device related adverse events or unanticipated adverse events. The majority of AEs reported in this study were mild or moderate in severity. The majority of SAEs were pulmonary and expected events as part of a lung resection surgery. Two patients died during the course of the study, one due to cardiac arrest and another due to multi-system organ failure; neither were device related or unanticipated.
The details of these clinical trial adverse events can be reviewed in the IFU supplied with the product an d also available at www.bd.com
Caution: Federal (USA) law restricts this device to sale by or on order of a licensed physician or properly licensed practitioner.
BD-79626
The Basics of the Progel™ Pleural Air Leak Sealant
Progel™ Pleural Air Leak Sealant (PALS) is a unique option that can help you address postoperative air leak complications. Progel™ PALS is clinically proven to seal pleural air leaks and reduce length of hospital stay.1
Progel™ PALS is a specialized sealant comprised of a proprietary combination of human serum albumin (HSA) and polyethylene glycol (PEG). The resulting hydrogel provides strength, flexibility and adherence to the visceral pleura.
Some benefits of the Progel™ Pleural Air Leak Sealant include:
- Variable spray patterns for targeted application
- Extended applicator spray tips
- Strength and flexibility
Optimal contact and adherence
Surgical Sealant Basics
Surgical sealants are used as leak barriers for fluids, like blood, urine, or even air. As an example, sealants may be used to patch a puncture located in the lung. Sealant devices might also be applied to tissue wounds as a hemostatic agent in order to control bleeding.
Progel, for example, is the only product that is FDA-approved as an adjunct for the treatment of pleural air leaks that occur during an open thoracotomy. This surgical sealant forms a very flexible hydrogel which is specifically designed for use on the lungs.
Surgical sealants can reduce postoperative air leaks and the time it takes to do a chest drain removal. For example, sealants have been known to be used to patch a puncture in the lung, as well potential in laparoscopy.
The two major types of surgical sealants of biologically derived tissue adhesives and sealants are fibrin glue and matrix protein adhesives. These can be effective in many applications, such as graft attachment, colon, vascular, and lung sealing. Since most fibrin and matrix-protein-based sealant products are derived from animal and human tissues, they are typically more expensive and have more limited availability when compared to synthetics like cyanoacrylates adhesives.
Cyanoacrylate, as well as various polymer hydrogels, represent the synthetic adhesives and sealants which have been proposed to make up for the weaker mechanical strength of the biologically derived glues.
The terms “adhesives” and “sealants” are often utilized interchangeably even though their
intended uses and functions are very different. An adhesive has the characteristics to allow for in situ polymerization which causes adherence of tissue-to-tissue, or tissue-to-non-tissue surfaces.
Generally, tissue adhesives are used to hold two sides of tissues together, supporting wound healing until the regenerated tissue has enough mechanical strength. Sealants, alternatively, can be used as a barrier to fluids leaking, like blood, urine, or air.
Hemostatic devices are typically used with sutures or staples during surgery in order to control excessive bleeding. Hemostatic agents stop bleeding mechanically or by augmenting the coagulation cascade. Alternatively, tissue sealants are products which bind to and close defects in tissues.
The Progel™ Pleural Air Leak Sealant Products
Products related to the Progel™ Pleural Air Leak Sealant include:
Progel: Results and Case Studies
Evaluated in a prospective, randomized, multi-center trial, Progel™ PALS was also shown to significantly improve clinical outcomes. When used as indicated, Progel™ PALS can effectively seal intraoperative air leaks and significantly reduce the incidence of postoperative air leaks.
Shown to reduce the length of hospitalization by 1.9 mean days, potentially minimizing associated complications and cost-of-care.
BD-79626