true
Support
Sales
1.844.8.BD.LIFE (1.844.823.5433)
Thank you for contacting our sales team!
A sales representive will get in touch with you shortly.
Ordering
1.770.784.6100
bardmedical.customerservice@crbard.com
Onsite Visiting
8195 Industrial BoulevardCovington, Georgia 30014United States
Customer Service
1.844.8.BD.LIFE (1.844.823.5433)
bardmedical.customerservice@crbard.com
Shipping a Product Back
8195 Industrial Boulevard, Covington, Georgia 30014, United States
BD Aptra™ Digital Endoscope System
When your choice is a single-use scope, you should expect enhanced image quality, a small outer diameter and maximum deflection.

- Overview
- Why Choose Single-Use?
- EIFU & Resources
一次性使用输尿管内窥镜导管与本公司的医用内窥镜图像处理器配合使用,用于进行输尿管及肾盂疾病检查、诊断或治疗中成像。不能与高频附件配用。
true
Learn more about our stone management solutions
Video Player is loading.
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
- In simulated testing, data shows that the average resolution on the BD Aptra™ Ureteroscope is better than the LithoVue™ ureteroscope at all conclusive target distances.*
- Camera module which produced an image resolution of 400 x 400 pixels.
*Based on resolution bench-top testing at varying distances. May not be indicative of actual clinical performance.
- The BD Aptra™ Ureteroscope has a 5˚ greater maximum deflection angle than the LithoVue™ ureteroscope.**
- Maximum deflection of 275˚ in two directions.
**Information for LithoVue™ excerpted from literature published by Boston Scientific.
- A 3.6 Fr. working channel, camera module, and two LEDs are all built into a tapered 7.4 Fr. tip.
- LEDs at the tip for enhanced illumination and overall image quality.
- Ergonomic handle design & optimized location of access port and power cord for easier handling.
- Two programmable buttons to control key functionalities (e.g. brightness, zoom) and up to 3 unique user profiles can be stored on the BD Aptra™ Image System.
Al-Balushi, K; Martin, N, et al. Comparative medico-economic study of reusable vs. single-use flexible ureteroscopes. Springer Nature. 2019.
Ofstead, C.L; Heymann, O.L; et al. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. American Journal of Infection Control. 2017.
Sooriakumaran, P.; Kaba, R.; et al. Evaluation of the mechanisms of damange to flexible ureteroscopes and suggestions for ureteroscope preservation. AJA. 2005.
Hennessey, D.B.; Fojecki, G.L; et al. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJUI. 2018.
Davis, N.F.; McGrath, S.; et al. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. Journal of Endourology. Vol 32, 3; March 2018.
Intended use
BD Aptra™ Digital Endoscope System is intended to be used by physicians to access, visualize, and perform procedures in the urinary tract and the kidney. The instrument enables delivery and use of accessories such as biopsy forceps, laser fibers, graspers and retrieval baskets at a surgical site.
Contraindications
Diagnostic or therapeutic ureteroscopy is contraindicated in people with an untreated urinary tract infection. Other contraindications to therapeutic ureteroscopy (e.g. lithotripsy, endopyelotomy, tumor therapy) are more numerous and can mirror those associated with the corresponding open surgical interventions. Patients on anticoagulants or with coagulopathies should be managed appropriately.
Warnings
• Do not use electromedical energy sources in the presence of flammable detergents, anesthetics, nitrous oxide (N2O), or oxygen.
• Consult the user manuals of all electromedical energy sources used with endoscopic instruments for appropriate instruments, warnings and cautions prior to use. Such sources of energy include electrical, electrohydraulic, electrosurgical, heat hydraulic, laser, light, pressure, sound, ultrasound and vacuum.
• Do not insert or advance the ureteroscope unless there is a clear live endoscopic view of the lumen through which the scope is being advanced (or confirm with visualization by other imaging modalities).
• During the procedure, if the live endoscopic image is lost, do not advance or insert the ureteroscope and do not insert, advance or actuate accessories.
• Do not use excessive force while advancing or withdrawing the scope. If resistance is felt during advancement or withdrawal of the scope, investigate the source of resistance and/or take remedial action if necessary.
• Do not force the distal tip of the ureteroscope against the sidewall of the ureter or renal pelvis.
• Do not use excessive force when advancing or withdrawing an accessory within the ureteroscope.
• When inserting or using accessories, maintain continuous visualization of the distal tip. Ensure that the distance between the distal tip of the ureteroscope and the object in view is greater than the ureteroscope’s minimum visible distance. Failure to do so may result in the accessories causing patient injury.
• Do not withdraw a laser fiber back into the ureteroscope while the laser is firing. Doing so may cause patient injury and/or scope damage.
• Do not look directly into the light emitted from the ureteroscope.
• Verify ground isolation when setting up and using accessories from different manufacturers prior to procedure.
• Do not open the handle of the ureteroscope.
• The ureteroscope is a single-use device and there are no serviceable parts. Do not repair damaged or non-operating ureteroscopes. Do not use the ureteroscope if damage is discovered or suspected.
• Do not excessively bend the flexible shaft or the articulating section of the ureteroscope.
• If damage to the ureteroscope occurs or it stops functioning during a procedure, stop using the ureteroscope immediately. See troubleshooting section for more information. Continue the procedure with a new ureteroscope, as appropriate.

Risk of Infection
Choose single-use and decrease the potential risk of infection post-procedure or other possible contamination associated with reprocessing reusable ureteroscopes.
A recent US study analyzed 16 fURS showing, despite validated disinfection procedures, there is no such risk with single-use fURS since a new ureteroscope is used for every patient.1

100% of the [reusable] fURS had visible irregularities and contamination by microbial growth, hemoglobin, a protein, or a chemical indicating the presence of living cells.2*
*Based on study results performed by Ofstead et al. with a sample size of n=16 ureteroscopes.

Unavailability of Reusables
Choosing single-use could help reduce canceled or rescheduled cases, lost revenue, wasted time and prolonged pain for the patient due to an unavailable ureteroscope.
Data suggests:
- Unavailability of reusable scopes is the number one reason for the cancellation of the procedure.1
- The average unavailability of reusable scopes is 200 days per year due to damages.1
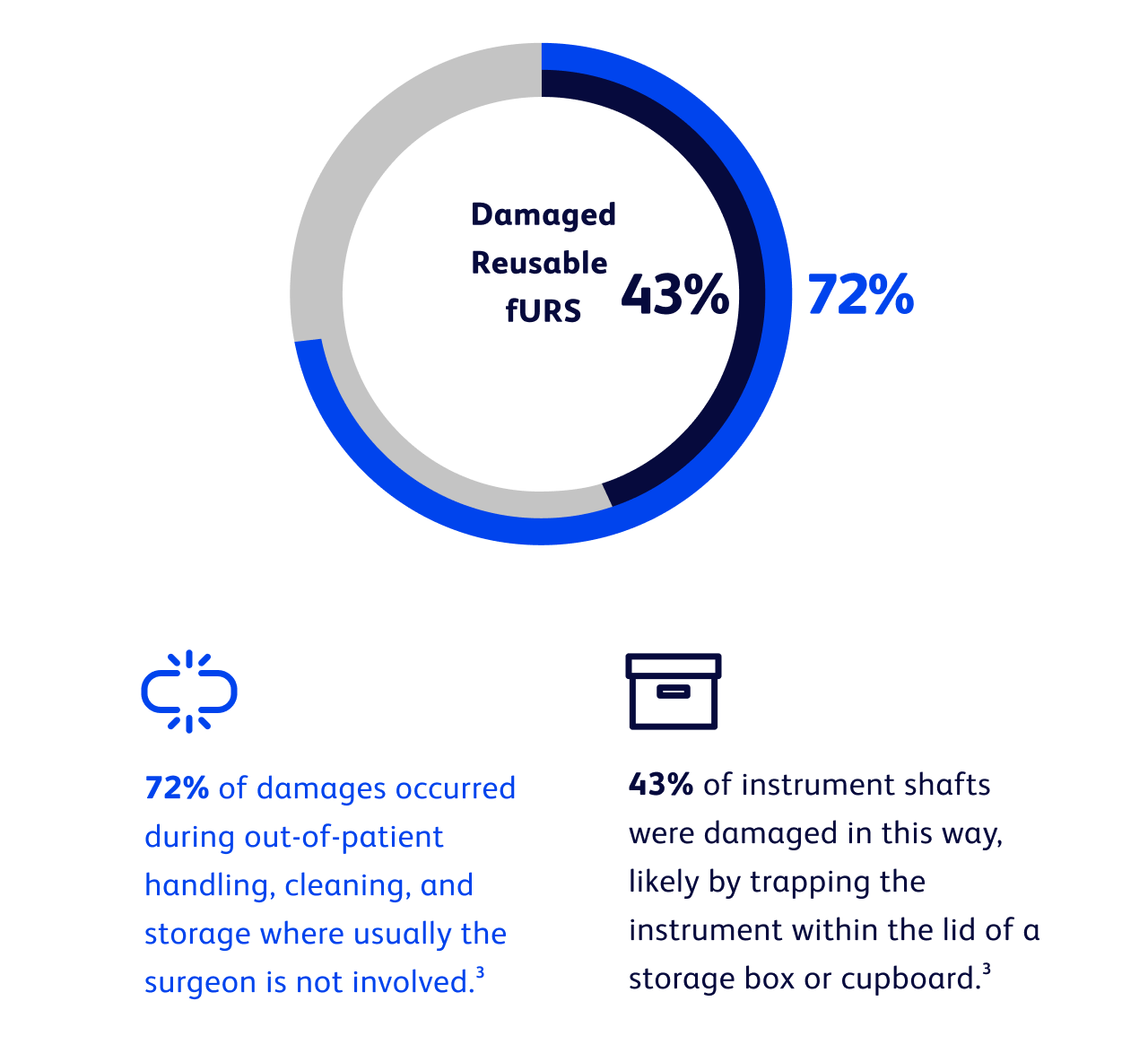
Unpredictable Failures
Choose single use, avoid performance degradation or scope failure due to reprocessing and sterilization:
- Significant issues associated with both fiber optic and digital reusable scope use = initial purchase cost, maintenance cost, performance degradation, poor durability. 4
- Flexible ureteroscopes are very delicate instruments notorious for limited durability and high costs associated with repairs.3
- Reusable scopes lose functionality over time—loss of flexion and deflection and, in fiber optic instruments, image quality—potentially affecting the outcome of stone surgery.4

In 1 year, 61% of reusable scopes were sent back to the manufacturer.3*
*Based on study results performed by Sooriakumaran, et al. with a sample size of n=78 ureteroscopes.
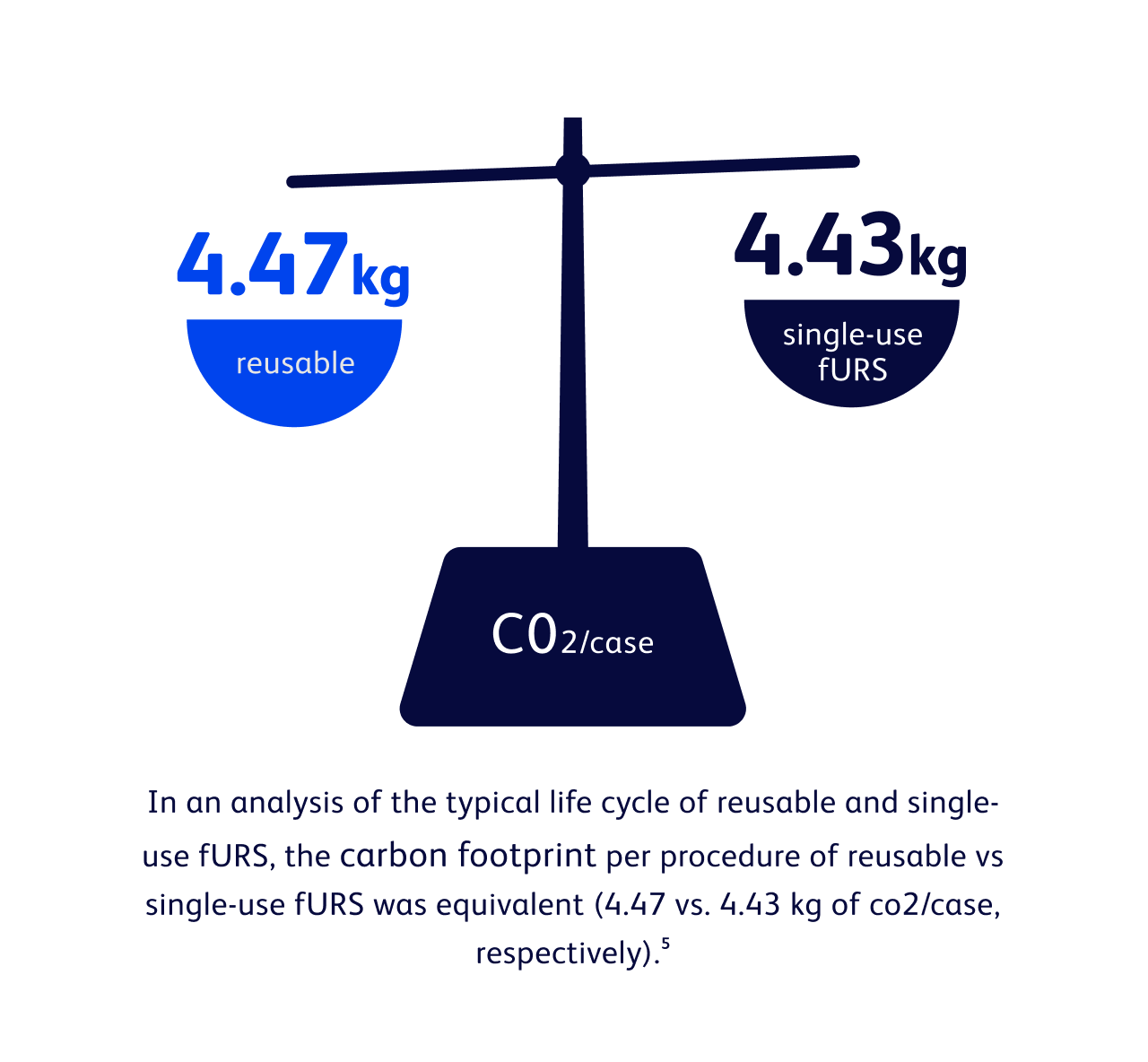
Environmental Concerns
Choose single-use, limit hospital staff exposure and reduce hospital waste.
- Single-use fURS do not require decontamination and sterilization1
- Personnel are not exposed to detergents or disinfectants1
- Reduction of hospital waste associated with high-level sterilization process1
1. Al-Balushi, K; Martin, N, et al. Comparative medico-economic study of reusable vs. single-use flexible ureteroscopes. Springer Nature. 2019.
2. Ofstead, C.L; Heymann, O.L; et al. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. American Journal of Infection Control. 2017.
3. Sooriakumaran, P.; Kaba, R.; et al. Evaluation of the mechanisms of damange to flexible ureteroscopes and suggestions for ureteroscope preservation. AJA. 2005.
4. Hennessey, D.B.; Fojecki, G.L; et al. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJUI. 2018.
5. Davis, N.F.; McGrath, S.; et al. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. Journal of Endourology. Vol 32, 3; March 2018.
Intended use
BD Aptra™ Digital Endoscope System is intended to be used by physicians to access, visualize, and perform procedures in the urinary tract and the kidney. The instrument enables delivery and use of accessories such as biopsy forceps, laser fibers, graspers and retrieval baskets at a surgical site.
Contraindications
Diagnostic or therapeutic ureteroscopy is contraindicated in people with an untreated urinary tract infection. Other contraindications to therapeutic ureteroscopy (e.g. lithotripsy, endopyelotomy, tumor therapy) are more numerous and can mirror those associated with the corresponding open surgical interventions. Patients on anticoagulants or with coagulopathies should be managed appropriately.
Warnings
• Do not use electromedical energy sources in the presence of flammable detergents, anesthetics, nitrous oxide (N2O), or oxygen.
• Consult the user manuals of all electromedical energy sources used with endoscopic instruments for appropriate instruments, warnings and cautions prior to use. Such sources of energy include electrical, electrohydraulic, electrosurgical, heat hydraulic, laser, light, pressure, sound, ultrasound and vacuum.
• Do not insert or advance the ureteroscope unless there is a clear live endoscopic view of the lumen through which the scope is being advanced (or confirm with visualization by other imaging modalities).
• During the procedure, if the live endoscopic image is lost, do not advance or insert the ureteroscope and do not insert, advance or actuate accessories.
• Do not use excessive force while advancing or withdrawing the scope. If resistance is felt during advancement or withdrawal of the scope, investigate the source of resistance and/or take remedial action if necessary.
• Do not force the distal tip of the ureteroscope against the sidewall of the ureter or renal pelvis.
• Do not use excessive force when advancing or withdrawing an accessory within the ureteroscope.
• When inserting or using accessories, maintain continuous visualization of the distal tip. Ensure that the distance between the distal tip of the ureteroscope and the object in view is greater than the ureteroscope’s minimum visible distance. Failure to do so may result in the accessories causing patient injury.
• Do not withdraw a laser fiber back into the ureteroscope while the laser is firing. Doing so may cause patient injury and/or scope damage.
• Do not look directly into the light emitted from the ureteroscope.
• Verify ground isolation when setting up and using accessories from different manufacturers prior to procedure.
• Do not open the handle of the ureteroscope.
• The ureteroscope is a single-use device and there are no serviceable parts. Do not repair damaged or non-operating ureteroscopes. Do not use the ureteroscope if damage is discovered or suspected.
• Do not excessively bend the flexible shaft or the articulating section of the ureteroscope.
• If damage to the ureteroscope occurs or it stops functioning during a procedure, stop using the ureteroscope immediately. See troubleshooting section for more information. Continue the procedure with a new ureteroscope, as appropriate.
Literature
Our wide range of documentation can help you understand, use and optimize our products.
Learn more
Videos
BD Aptra™ collection of videos on our offerings gives you information you can use to continue striving for excellence.
Learn More
Al-Balushi, K; Martin, N, et al. Comparative medico-economic study of reusable vs. single-use flexible ureteroscopes. Springer Nature. 2019.
Ofstead, C.L; Heymann, O.L; et al. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. American Journal of Infection Control. 2017.
Sooriakumaran, P.; Kaba, R.; et al. Evaluation of the mechanisms of damange to flexible ureteroscopes and suggestions for ureteroscope preservation. AJA. 2005.
Hennessey, D.B.; Fojecki, G.L; et al. Single-use disposable digital flexible ureteroscopes: an ex vivo assessment and cost analysis. BJUI. 2018.
Davis, N.F.; McGrath, S.; et al. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. Journal of Endourology. Vol 32, 3; March 2018.
Intended use
BD Aptra™ Digital Endoscope System is intended to be used by physicians to access, visualize, and perform procedures in the urinary tract and the kidney. The instrument enables delivery and use of accessories such as biopsy forceps, laser fibers, graspers and retrieval baskets at a surgical site.
Contraindications
Diagnostic or therapeutic ureteroscopy is contraindicated in people with an untreated urinary tract infection. Other contraindications to therapeutic ureteroscopy (e.g. lithotripsy, endopyelotomy, tumor therapy) are more numerous and can mirror those associated with the corresponding open surgical interventions. Patients on anticoagulants or with coagulopathies should be managed appropriately.
Warnings
• Do not use electromedical energy sources in the presence of flammable detergents, anesthetics, nitrous oxide (N2O), or oxygen.
• Consult the user manuals of all electromedical energy sources used with endoscopic instruments for appropriate instruments, warnings and cautions prior to use. Such sources of energy include electrical, electrohydraulic, electrosurgical, heat hydraulic, laser, light, pressure, sound, ultrasound and vacuum.
• Do not insert or advance the ureteroscope unless there is a clear live endoscopic view of the lumen through which the scope is being advanced (or confirm with visualization by other imaging modalities).
• During the procedure, if the live endoscopic image is lost, do not advance or insert the ureteroscope and do not insert, advance or actuate accessories.
• Do not use excessive force while advancing or withdrawing the scope. If resistance is felt during advancement or withdrawal of the scope, investigate the source of resistance and/or take remedial action if necessary.
• Do not force the distal tip of the ureteroscope against the sidewall of the ureter or renal pelvis.
• Do not use excessive force when advancing or withdrawing an accessory within the ureteroscope.
• When inserting or using accessories, maintain continuous visualization of the distal tip. Ensure that the distance between the distal tip of the ureteroscope and the object in view is greater than the ureteroscope’s minimum visible distance. Failure to do so may result in the accessories causing patient injury.
• Do not withdraw a laser fiber back into the ureteroscope while the laser is firing. Doing so may cause patient injury and/or scope damage.
• Do not look directly into the light emitted from the ureteroscope.
• Verify ground isolation when setting up and using accessories from different manufacturers prior to procedure.
• Do not open the handle of the ureteroscope.
• The ureteroscope is a single-use device and there are no serviceable parts. Do not repair damaged or non-operating ureteroscopes. Do not use the ureteroscope if damage is discovered or suspected.
• Do not excessively bend the flexible shaft or the articulating section of the ureteroscope.
• If damage to the ureteroscope occurs or it stops functioning during a procedure, stop using the ureteroscope immediately. See troubleshooting section for more information. Continue the procedure with a new ureteroscope, as appropriate.
true





