Antimicrobial Resistance
Our future depends on what we do today.

- About
- Prevention
- Awareness
- Resources
Since the introduction of penicillin in 1942, antimicrobials have transformed the treatment of infections and saved millions of lives. But organisms “resistant” to penicillin were noticed from almost the very beginning. Now, decades of misuse and outdated guidelines have driven a rise in the organisms that are resistant to these lifesaving drugs.
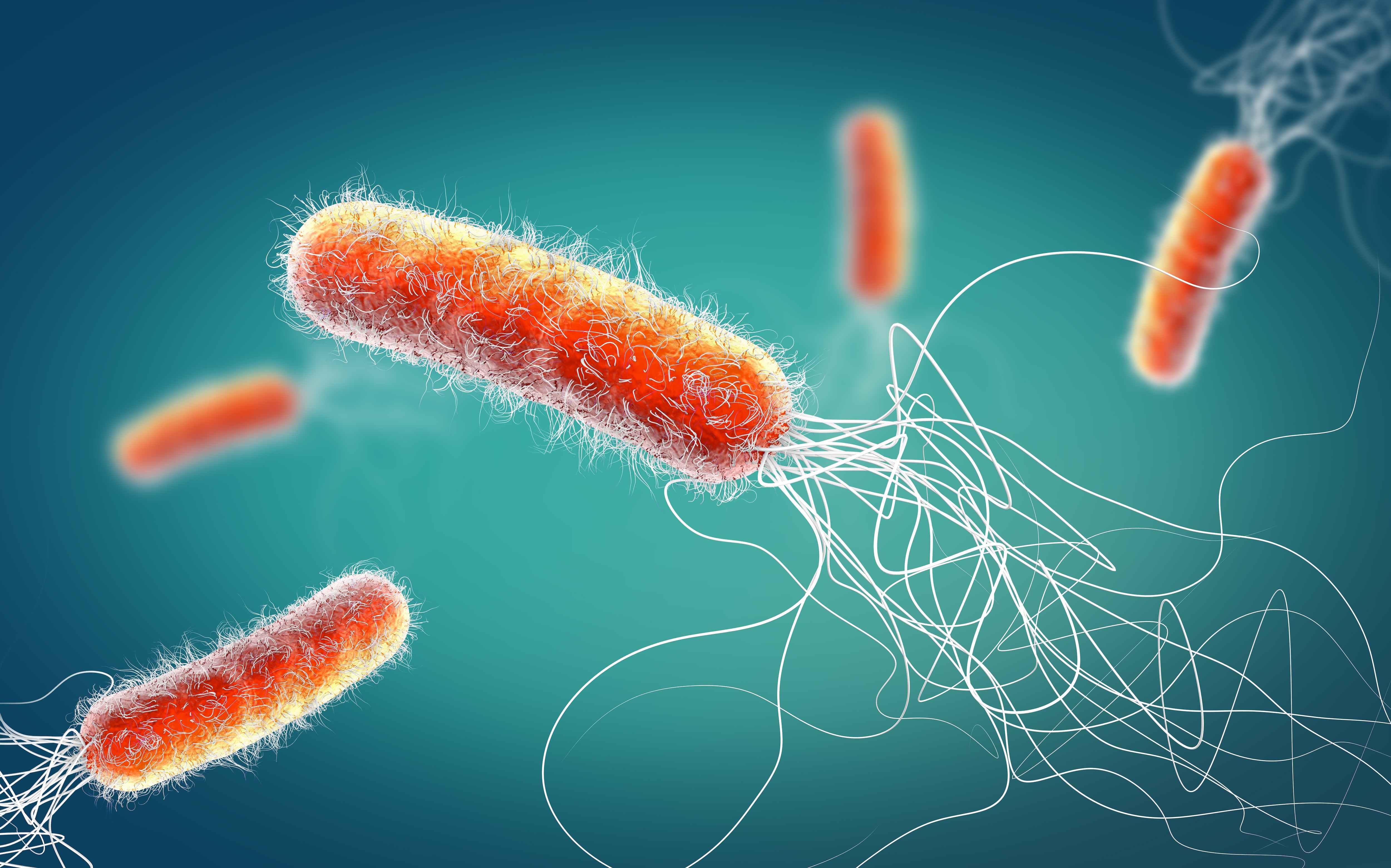
Antimicrobial resistance (AMR) is the ability of miroorganisms (including bacteria, fungi, viruses, etc.) to nullify the effects of antimicrobial drugs, resulting in these drugs becoming ineffective.1,2 AMR can affect anyone, of any age, in anycountry. 1
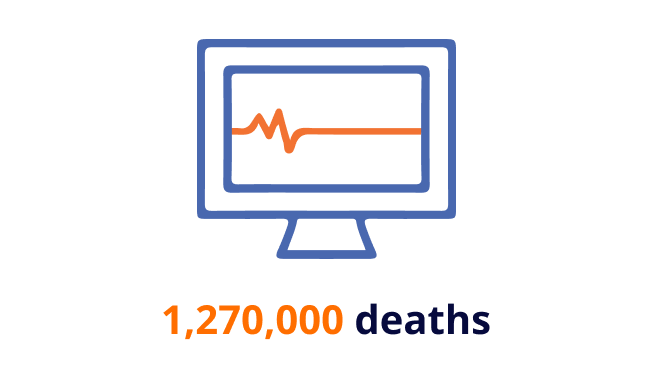
Today, AMR is one of the world’s greatest health threats, causing over 1 million deaths each year, and that number is growing.3
The severity has prompted the World Health Organization (WHO) to declare AMR as one of the top 10 global public health threats facing humanity.4
As the problem continues, common medical procedures will become increasingly life-threatening. Left unabated, the problem will grow exponentially, literally threatening every person on earth.
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines designed to kill them.
As a result of drug resistance, infections become harder to treat, increasing the risk of disease spread, severe illness and death.
1. High number of bacteria
Whenever there is a high number of bacteria, a small number of them are resistant to antibiotics.
2. Antibiotics kill bacteria
When taken, antibiotics kill bacteria causing the illness but they also kill the good bacteria that protect the body from infection.
3. Resistant bacteria grow and multiply
The resistant bacteria can now grow and multiply without competition.
4. Transfer of resistance
Some bacteria can transfer their resistance to antibiotics to other bacteria, which can cause more problems.

If left unabated, the effects of AMR could be worse than COVID-19. 6,11 Future projections suggest that AMR could result in millions of deaths and trillions of dollars in lost global production. 7
As the problem continues, common medical procedures will become increasingly life-threatening. The problem can grow exponentially, literally threatening every person on earth.
The Global Fight Against Antimicrobial Resistance
From Broadview Pictures @2022. Silent Pandemic was produced by Broadview Pictures in co-production with ZDF and in cooperation with ARTE. All rights reserved. Used under agreement.
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button.
Our global public health efforts seek to expand access and drive capacity-building through partnerships with leading organizations and governments.
We engage in advocacy with governments, funders and health agencies to advance innovations to address the world’s leading public health needs, including drug-resistant infections.
We possess important capabilities that are instrumental in containing AMR. We offer a wide range of medical products, platforms and offerings that can be used to prevent the spread of infection in healthcare facilities, such as diagnostic systems to screen, test and diagnose infection, including drug-resistant strains, as well as state-of-the-art surveillance and reporting capabilities to monitor, track and predict AMR outbreaks.
Enabled by our innovative programs and technologies, BD teams across the globe are directly engaging AMR leaders in government, academia and professional societies to strengthen AMR awareness, health systems, capacities and infection prevention and diagnostic practices.
BD is leveraging its extensive global capabilities to meaningfully engage around 5 key strategies to reduce the burden of drug-resistant infections.

Infection prevention and control practices and guidelines

Surveillance
Identifying emerging threats and developing an effective response plan is one of the key leverage points in battling AMR.
We must take action against drug-resistant infections, TOGETHER!
New and Newsworthy
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
References
1. World Health Organization. Antimicrobial resistance fact sheet. http://www.who.int/mediacentre/factsheets/fs194/en/. Accessed November 28, 2017.
2. Centers for Disease Control and Prevention. About antimicrobial resistance. https://www.cdc.gov/drugresistance/about.html. Accessed May 12, 2017.
3. Institute for Health Metrics and Evaluation. The latest estimates of global anti-microbial resistance showurgent policy action is needed to save lives. https://www.healthdata.org/news-release/latest-estimatesglobal-anti-microbial-resistance-show-urgentpolicyactionneededsave#:~:text=An%20estimated%204.95 %20million%20people,young%20children%20are%20particularly%20affected. Accessed February 8, 2022.
4. World Health Organization. Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-toglobal-health-in-2019. Accessed February 8, 2022.
5. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629-655.
6. Centers for Disease Control and Prevention. More people in the United States dying from antibioticresistant infections than previously estimated. https://www.cdc.gov/media/releases/2019/p1113-antibioticresistant. html; Accessed June 23, 2022.
7. O’Neill J. Antimicrobial resistance: tackling a crisis for the health and wealth of nations. https://amrreview.
org/sites/default/files/AMR%20Review%20Paper%20%20Tackling%20a%20crisis%20
for%20the%20health%20and%20wealth%20of%20nations_1.pdf. Accessed February 8, 2022.
8. Smith R, Coast J. The true cost of antimicrobial resistance. BMJ. 2013;346:f1493.
9. World Bank. By 2050, drug-resistant infections could cause global economic damage on par with 2008
financial crisis, http://www.worldbank.org/en/news/press-release/2016/09/18. Accessed October 12, 2017.
10. Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA,
2007–09. J Antimicrob Chemother. 2013;69(1):234-240.
11. Ukuhor H. The interrelationships between antimicrobial resistance, COVID-19, past, and future
pandemics. J Infect Public Health. 2021;14(1):53-60.
Infection prevention and control initiatives work to prevent the spread of infections caused by multidrug-resistant bacteria, reduce the need for antibiotics and help curb the emergence of antibiotic resistance.
Infection control practices, from simple handwashing to global vaccination and the use of effective infection prevention measures, are key tools to combat AMR. Preventing drug-resistant infections reduces the use of antibiotics and improves patient outcomes.
SOURCES OF INFECTION
Standardize and simplify your medication management process
Your medication management solution should be a reliable source for the information and medications needed as patient conditions evolve. Our solutions standardize and simplify your medication management process, reducing the risk for error and inefficiency. BD connected technologies work together with your EMR to provide added safety for your patients and confidence for your clinicians.
Beyond the EHR: Best Practices in Enterprise Medication Management
Streamline operations with actionable insights
Delivering industry-leading patient care doesn’t need to strain financial resources and put undue pressure on your staff. Connected Medication Management brings together disparate systems so you can achieve a consistent view across your sites of care. You can free your staff to get back to working at the top of their licenses, allowing them to focus on what matters most—delivering outstanding patient care.
Unite disparate systems and gain visibility
When your data is scattered, your operations can be too. Connected Medication Management leverages your EMR to create a comprehensive view of inventory on hand. That means managing fewer databases and gaining visibility so you can make valuable impacts on workflows across your organization and minimize medication diversion and adverse drug events. By having connected systems and bidirectional data exchange, predictive analytics can inform critical decision-making about care needs, help control carrying costs and avoid wasted inventory.
Partnering on prevention
At BD, we are leveraging our expertise in diagnostics, vascular access, surgical preparation and critical care to support hospitals’ infection prevention and control programs. BD is committed to helping clinicians improve patient outcomes through the standardization of care and adherence to best practices.
SHEA: In support of the infection prevention efforts of the Society for Healthcare Epidemiology of America (SHEA), BD provides an educational grant for the “Prevention Course in HAI Knowledge and Control”—a free educational resource to keep frontline providers, their families, and patients safe.
International Collaboration: BD has worked with national governments in multiple countries, including the United States, China, Kenya, Cambodia, and India, via public-private partnerships to improve hospitals’ capabilities with infection prevention and control.
Educational Publication Partnerships: BD leverages expertise from internal clinical pharmacists, infectious disease physicians and industry-leading data scientists to produce more than 500 unique analytic tool sets, resulting in publications informing infection prevention guidelines.
Working together to improve processes: BD partners with clinicians in addressing vascular access-related complications by identifying gaps in their current vascular access process.
BD Product Solutions
Systematic infection prevention and control procedures reduce the frequency and extent of healthcare-associated infections (HAIs) and the spread of antimicrobial-resistant organisms. Comprehensive product and service offerings from BD help clinicians improve patient outcomes through the standardization of care and adherence to best practices.
-
Vascular access management is vital to help reduce complications and infections, and to improve patient outcomes.
-

Preoperative skin preparation is an important step in helping to limit surgical wound contamination and prevent infection.
-

Products and kits designed to reduce variability or improve compliance in critical care practice.
We must take action against drug-resistant infections, TOGETHER!
References
- World Health Organization. Antimicrobial resistance fact sheet. http://www.who.int/mediacentre/factsheets/fs194/en/. Accessed November 28, 2017.
- Centers for Disease Control and Prevention. About antimicrobial resistance. https://www.cdc.gov/drugresistance/about.html. Accessed May 12, 2017.
- Institute for Health Metrics and Evaluation. The latest estimates of global anti-microbial resistance show urgent policy action is needed to save lives. https://www.healthdata.org/news-release/latest-estimates-global-anti-microbial-resistance-show-urgent-policyactionneededsave#:~:text=An%20estimated%204.95%20million%20people,young%20children%20are%20particularly%20affected. Accessed February 8, 2022.
- World Health Organization. Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-toglobal-health-in-2019. Accessed February 8, 2022.
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet.2022;399(10325):629-655.
- Centers for Disease Control and Prevention. More people in the United States dying from antibiotic-resistant infections than previously estimated. https://www.cdc.gov/media/releases/2019/p1113-antibiotic-resistant.html; Accessed June 23, 2022.
- O’Neill J. Antimicrobial resistance: tackling a crisis for the health and wealth of nations. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf. Accessed February 8, 2022.
- Smith R, Coast J. The true cost of antimicrobial resistance. BMJ. 2013;346:f1493.
- World Bank. By 2050, drug-resistant infections could cause global economic damage on par with 2008 financial crisis, http://www.worldbank.org/en/news/press-release/2016/09/18. Accessed October 12, 2017.
- Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chemother. 2013;69(1):234-240.
- Ukuhor H. The interrelationships between antimicrobial resistance, COVID-19, past, and future pandemics. J Infect Public Health. 2021;14(1):53-60.
Patients: what you can do to combat AMR
- Only use antibiotics when prescribed by a certified health professional
- Always finish antibiotic prescriptions
- Never share or use leftover antibiotics
- Don't take antibiotics for viruses, such as the cold or flu (antibiotics only work on bacteria)
- Prevent infections by regularly washing hands, preparing food hygienically, avoiding close contact with sick people and keeping vaccinations up to date
Healthcare settings are high-risk environments for the spread of organisms that cause infections.
- 7% to 10% of hospitalized patients and 33% of patients in intensive care units contract at least one healthcare-associated infection.1,2
- 25% of healthcare-associated infections in long-term acute care settings are caused by antibiotic-resistant bacteria.1
Recommendation:
All healthcare facilities need to implement sufficient cleaning and disinfection protocols and properly dispose of biohazardous waste in order to reduce the potential for spreading healthcareassociated infections. Improving the quality of these practices and use of advanced decontamination technologies are needed.3
1Review on Antimicrobial Resistance. Infection prevention, control, and surveillance: Limiting the development and spread of drug-resistance. London, England: Wellcome Trust and HM Government; 2016.
2 World Health Organization. Report on the burden of endemic health care-associated infection worldwide. Geneva, Switzerland: World Health Organization; 2011.
3 Boyce JM. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob Resist Infect Control. 2016;5:10.
Healthcare workers and other caregivers can be a source of infection when appropriate prevention and control measures are not taken.
- Only 40% of healthcare workers adhere to recommended handwashing practices, although self-reported rates are nearly 100%.1
Recommendation:
Consistent hand hygiene is the single most important infection prevention and control intervention in the healthcare setting.4 Antimicrobial hand sanitization products are effective means of hand hygiene that decrease the risk of infection in healthcare settings.5
1 Review on Antimicrobial Resistance. Infection prevention, control, and surveillance: Limiting the development and spread of drug-resistance. London, England: Wellcome Trust and HM Government; 2016.
4 Pittet D, Allegranzi B, Sax H, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6(10):641–652.
5 Weinstein RA. Controlling antimicrobial resistance in hospitals: infection control and use of antibiotics. Emerg Infect Dis. 2001;7(2):188–192.
Medical devices and surgical procedures are potential sources of infection.
- 17% of central-line, 14% of surgical-site and 10% of catheter-associated infections are caused by antibiotic-resistant bacteria.6
- Catheter-related bloodstream infections account for 10% to 20% of hospital-acquired infections in the UK and are associated with extended intensive care unit stay and increased mortality.7
Recommendation:
Training guidelines for proper central-line and intravenous catheter use need to be followed.6 Appropriate antiseptic agents, skin preparation and sterile dressings minimize the risk of surgical-site infections.8 Closed needleless intravenous access ports reduce the risk of microbes entering the patient’s bloodstream.9
6 Centers for Disease Control and Prevention. Making health care safer: Protect patients from antibiotic resistance. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2016.
7 Gahlot R, Nigam C, Kumar V, Yadav G, Anupurba S. Catheter-related bloodstream infections. Int J Crit Illn Inj Sci. 2014;4(2):162–167.
8 Centers for Disease Control and Prevention. Basic Infection Control and Prevention Plan for Outpatient Oncology Settings. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2011.
9 Blake M. Update: Catheter-related bloodstream infection rates in relation to clinical practice and needleless device type. Can J Infect Control. 2008;23(3):156–160, 162.
Patients can be a source of transmission of infectious bacteria to caregivers, to other patients and often, to themselves.
- Up to 30% of individuals carry Staphylococcus aureus, a potentially harmful bacterium.10
- Up to 7.2% of hospitalized patients can carry methicillin-resistant Staphylococcus aureus (MRSA), a strain of the bacteria resistant to commonly used antibiotics.11
- Patients' own bacteria cause the majority of catheter-related bloodstream infections and a large proportion of surgical-site infections.12,13
Recommendation:
Health systems and healthcare facilities need to establish protocols to screen patients for harmful bacteria using diagnostic tests where available. If patients are found positive for harmful bacteria, then actions need to be taken by healthcare facilities and providers. The spread of infections can be reduced through awareness of outbreaks, appropriate treatment, isolation of patients with resistant microorganisms, adherence to recommended infection control practices and use of personal protective devices and equipment.14
10 Wertheim HF, Melles DC, Vos MC, et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005;5(12):751–762.
11 Davis KA, Stewart JJ, Crouch HK, Florez CE, Hospenthal DR. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis. 2004;39(6):776–782.
12 Maki DG. Infections caused by intravascular devices used for infusion therapy: Pathogenesis, prevention, and management. In: Bisno AL, Waldvogel FA, eds. Infections Associated with Indwelling Medical Devices. 2nd ed. Washington, DC: American Society for Microbiology; 1994:151–212.
13 Wenzel RP. Minimizing surgical-site infections. N Engl J Med. 2010;362(1):75–77.
14 Siegel JD, Rhinehart E, Jackson M, Chiarello L, Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2007.
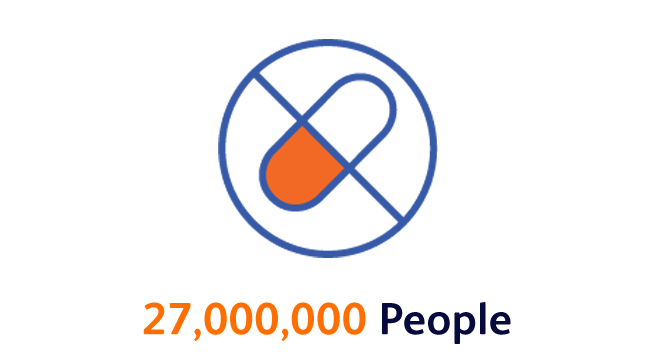
Upon initial examination, patients are commonly prescribed antibiotics that are either unnecessary or ineffective.
- At least 30% of antibiotics prescribed in the United States are unnecessary.15
- Most infections in developing countries are treated empirically without the benefit of diagnostic tests, leading to even higher rates of unnecessary antibiotic use.16
Recommendation:
When assessing the need for antibiotic therapy, clinicians need to combine the observed symptoms and signs with diagnostic tests for direct or indirect evidence of an infection and adherence to clinical practice guidelines for diagnosis and treatment.17 Countries and healthcare facilities with low resources will need support to increase access to and use of cost-effective diagnostic tests.
15 Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011. JAMA. 2016;315(17):1864–1873.
16 Sosa AJ, Byarugaba DK, Amábile-Cuevas CF, et al, eds. Antimicrobial Resistance in Developing Countries. New York, NY: Springer; 2010.
17 Boyles TH, Wasserman S. Diagnosis of bacterial infection. S Afr Med J. 2015;105(5):419–421.
Patients with viral infections are commonly treated with antibiotics, even though viruses do not respond to antibiotic therapy. Diagnostic tests that can distinguish between viral and bacterial infections are either unavailable or not widely used, especially in developing countries.16
- Most upper respiratory tract infections are caused by viruses, yet 50% of patients with these infections receive antibiotics.18
Recommendation:
Use of diagnostic tests that enable evidence-based prescribing practices needs to become the standard of care. Point-of-care diagnostics that rapidly confirm the type and source of infection can reduce inappropriate over-prescription of antibiotics.16
16 Sosa AJ, Byarugaba DK, Amábile-Cuevas CF, et al, eds. Antimicrobial Resistance in Developing Countries. New York, NY: Springer; 2010.
18 Caliendo AM, Gilbert DN, Ginocchio CC, et al. Better tests, better care: Improved diagnostics for infectious diseases. Clin Infect Dis. 2013;57(suppl 3):S139–S170.
Antibiotic susceptibility testing is important to confirm whether the selected antimicrobial agent is effective or is associated with resistance,19,20 but this testing is uncommon in many developing countries.20
- In the poorest countries, < 1% of patients are treated at clinical facilities that have diagnostic microbiology laboratories.16
Recommendation:
Susceptibility testing is recommended to determine whether a patient will respond to antibiotic therapy. All countries, including developing countries, need to improve access to basic microbiology laboratory testing and facilities. New automated diagnostics that provide rapid and cost-effective results are needed.19
16 Sosa AJ, Byarugaba DK, Amábile-Cuevas CF, et al, eds. Antimicrobial Resistance in Developing Countries. New York, NY: Springer; 2010.
19 Jorgensen JH, Ferraro MJ. Antimicrobial susceptibility testing: A review of general principles and contemporary practices. Clin Infect Dis. 2009;49(11):1749–1755.
20 Laxminarayan R, Bhutta Z, Duse A, et al. Drug Resistance. In: Jamison DT, Breman JG, Measham AR, et al, eds. Disease Control Priorities in Developing Countries. 2nd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2006:1031–1051.
Access to antibiotics for patients who need them is essential, yet prescribing practices vary globally, including over-the-counter access in some countries.
- In developing countries patients often present with advanced infections, requiring urgent treatment with antibiotics. Expanded access is needed in certain populations, such as treating children for pneumonia. Health systems need to balance these essential access needs with reducing the excessive overuse of antibiotics that occurs in all countries.
Recommendation:
Effective antibiotic stewardship and consistent prescribing practices are needed on a global basis. Initiatives to strengthen national laboratory systems, including expansion of laboratory technician workforces and higher access to simple cost-effective rapid diagnostic tests in remote areas, need to be prioritized, funded and supported by governments, public health agencies, foundations and the private sector.16
16 Sosa AJ, Byarugaba DK, Amábile-Cuevas CF, et al, eds. Antimicrobial Resistance in Developing Countries. New York, NY: Springer; 2010.
Surveillance is key to infectious disease management, but it remains underresourced in many countries.
- Due to the lack of coordination and information sharing, gaps exist in antimicrobial consumption and resistance in many regions of the world.21
Recommendation:
Surveillance tools need to be used to assimilate information generated by a variety of sources in order to streamline identification of patients who have acquired an infection and may require antimicrobial therapy. The near real-time availability of these data can enable clinicians to optimize treatment decisions and antimicrobial use.
21 World Health Organization. Antimicrobial resistance: global report on surveillance 2014. Geneva, Switzerland: World Health Organization; 2014.
Thorough surveillance can reveal the presence of resistant microorganisms and identify trends and outbreaks.
- In many regions of the world, poor laboratory capacity, infrastructure and data management prevent effective surveillance.22
Recommendation:
Effective surveillance efforts need to include an early warning system to detect emergent pathogens, resistant clusters and unusual infectious disease events so action can be taken to prevent or control an outbreak.
22 World Health Organization. Worldwide country situation analysis: response to antimicrobial resistance. Geneva, Switzerland: World Health Organization; 2015.
Many areas of the world have access to laboratory data, but the data are not in a format suitable for optimizing surveillance efforts and timely therapy selection.23
- Major gaps exist in surveillance data, and treatment guided by such limited data can increase antimicrobial resistance.21
Recommendation:
Continuous monitoring of appropriate antimicrobial prescribing is necessary to optimize antimicrobial therapy and patient outcomes. Patient diagnostic information, combined with resistance trends and timely data distribution to healthcare providers, facilitates effective antimicrobial treatment decision-making.23
21 World Health Organization. Antimicrobial resistance: global report on surveillance 2014. Geneva, Switzerland: World Health Organization; 2014.
23 World Health Organization. Surveillance standards for antimicrobial resistance. Geneva, Switzerland: World Health Organization, 2002.
Antimicrobial consumption and resistance data can guide local, regional and national interventions.
- Most developing countries do not have systems for monitoring antimicrobial resistance and consumption or evaluating the effect of interventions.24
Recommendation:
Robust and comprehensive infection control practices need to include measuring the impact of interventions and the appropriateness of antimicrobial prescribing. Public health authorities need to support infrastructure that promotes transmission of antimicrobial consumption and infection data to facilitate local, regional and national surveillance efforts.
24 World Health Organization. Community-based surveillance of antimicrobial use and resistance in resource-constrained settings: report on five pilot projects. Geneva, Switzerland: World Health Organization; 2009.
US Centers for Disease Control and Prevention (CDC)
-
10 facts on antimicrobial resistance
-
Antimicrobial Resistance Aide-memoire
-
Antimicrobial Resistance Fact sheet
-
Antimicrobial Resistance National Action Plans
-
Antimicrobial Resistance Newsletters
-
Antimicrobial Resistance Programme Page
-
GLASS documents and tools
-
Global Action Plan on Antimicrobial Resistance
-
UN high-level meeting on antimicrobial resistance
-
Worldwide country situation analysis


![<p><b>Common infections are know killing hunderds of thousands of people</b> every year because bacteria have become resistant to treatment. This includes historically treatable illnesses, such as pneumonia, healthcare-associated infections (HAIs) and foodbrone ailments.<sup>5[lancet]</sup></p>](/content/dam/bd-assets/bd-com/en-us/images/solutions/antimicrobial-resistance/Common_Infections.png)





















 Infection Prevention and Control
Infection Prevention and Control



